Lung Abscess in Children
Lung Abscess in children is a serious but uncommon condition where a localized area of the lung becomes filled with pus due to severe infection and tissue destruction. It often develops as a complication of Pneumonia. Early identification and appropriate treatment are essential to prevent long-term lung damage and complications.
Aetiology & Underlying Causes
A Lung Abscess usually occurs due to infection by bacteria that cause lung tissue destruction and necrosis. The pus-filled cavity typically forms when the body attempts to wall off the infection.
Common Causative Organisms
- Staphylococcus aureus (including MRSA)
- Streptococcus pneumoniae
- Group A Streptococcus
- Anaerobic bacteria (common in aspiration)
- Klebsiella pneumoniae and other Gram-negative bacteria
- Less commonly: Mycobacterium tuberculosis and fungal infections in immunocompromised children
Risk Factors
- Complicated or untreated Pneumonia
- Aspiration due to neurological disorders, swallowing difficulty, reflux, or seizures
- Congenital lung malformations
- Immune deficiency disorders
- Severe viral infection predisposing to secondary bacterial infection
Clinical Presentation
Symptoms of Lung Abscess may resemble severe or non-resolving Pneumonia. Key clinical features include:
- Persistent fever lasting more than 7–10 days
- Cough (may be productive with foul-smelling sputum)
- Breathing difficulty or fast breathing
- Chest pain
- Poor appetite, weight loss and fatigue
- Failure to improve with routine antibiotic therapy
- In severe cases: sepsis, anemia or clubbing (late sign)
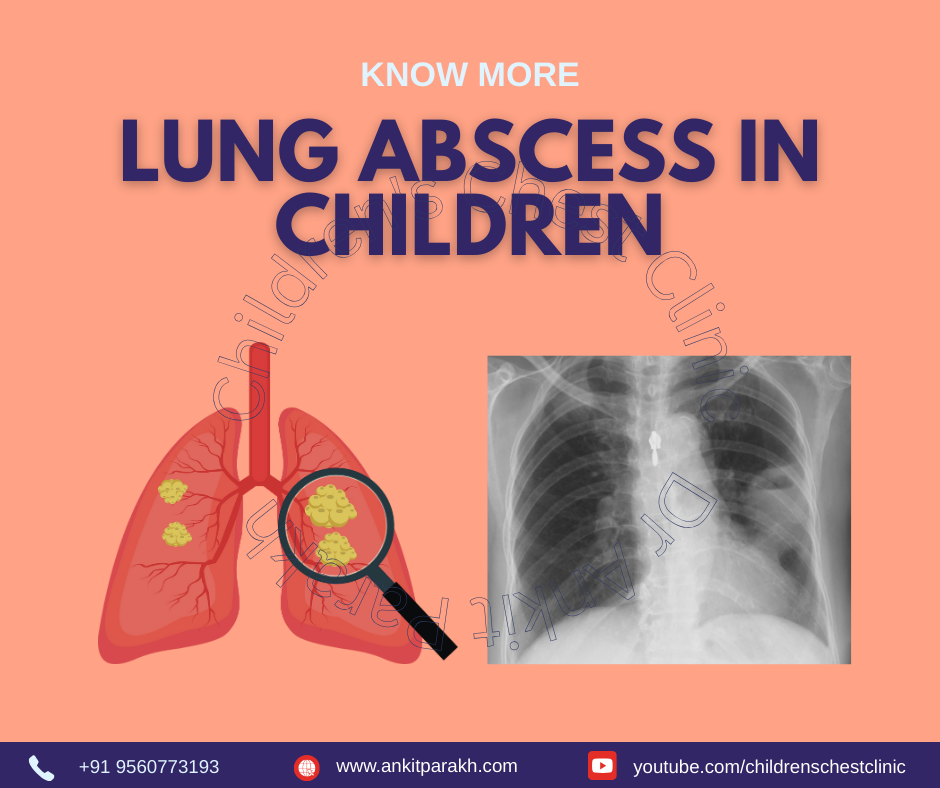
Investigations
Diagnostic Tests
- Chest X-ray – may show a cavity with air-fluid level
- Chest CT scan – confirms abscess location, size and complications
- Ultrasound chest – helpful when pleural involvement is suspected
- Blood tests – CBC, CRP, ESR, blood culture
- Sputum culture or bronchoalveolar lavage to identify pathogens
- Immunological workup if recurrent or non-resolving
Treatment & Management
1. Antibiotic Therapy
- Prolonged intravenous antibiotics targeted against common organisms
- Switch to oral antibiotics after clinical improvement
- Duration typically 4–6 weeks
- Covers anti-staphylococcal agents and anaerobic organisms
2. Supportive Care
- Adequate hydration & nutrition
- Oxygen support if required
- Chest physiotherapy for airway clearance
3. Drainage & Interventions
Most children respond to medical treatment. However, intervention may be needed if:
- No response to antibiotics
- Large abscess compressing the lung
- Rupture into pleural cavity
4. Follow-Up
- Repeat imaging to confirm healing
- Monitor lung function in prolonged cases
Complications
- Empyema
- Bronchopleural fistula
- Massive hemoptysis
Prevention
- Timely and appropriate treatment of Pneumonia
- Prevention of aspiration in high-risk children
- Vaccination including pneumococcal and influenza vaccines
Conclusion
Lung Abscess in children is a serious complication of Pneumonia requiring prompt diagnosis and prolonged antibiotic therapy. With early recognition and expert management by a Pediatric Pulmonologist, most children recover completely without long-term complications.