Vascular Airway Compression in Children
Vascular Airway Compression in children is an important yet often under-recognized cause of persistent breathing difficulties.
It occurs when abnormal positioning or enlargement of blood vessels compresses the trachea or bronchi, leading to airway obstruction.
Early identification and appropriate intervention are critical to prevent long-term complications.
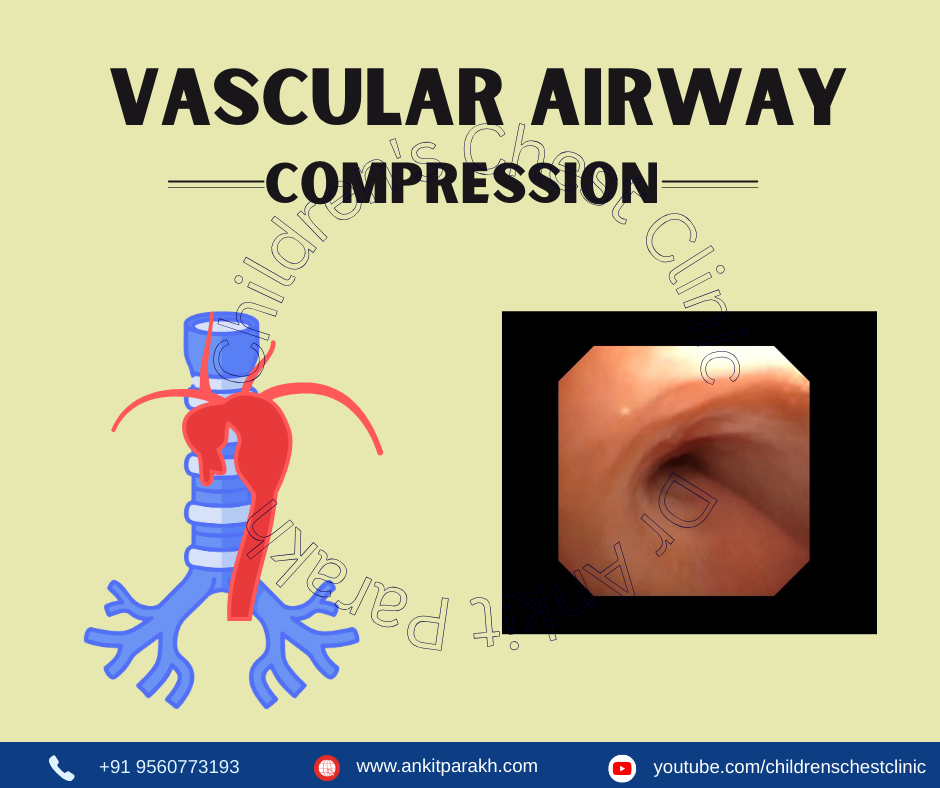
What is Vascular Airway Compression?
Vascular Airway Compression refers to the narrowing of the airway due to pressure from surrounding blood vessels.
Common causes include:
- Vascular rings (e.g., double aortic arch, right aortic arch with aberrant left subclavian artery)
- Pulmonary artery sling
- Dilated pulmonary arteries or aorta due to congenital heart disease
These conditions can significantly affect airflow, especially in infants and young children,
leading to recurrent respiratory symptoms.
Clinical Presentation
Symptoms often resemble asthma or recurrent respiratory infections, making diagnosis challenging. Common symptoms include:
- Stridor (noisy breathing)
- Persistent wheezing not responding to bronchodilators
- Barky cough or chronic cough
- Breathing difficulty during feeding or crying
- Recurrent pneumonias
- Apnea or cyanosis spells
- Failure to thrive in severe cases
Symptoms are usually worse during upper respiratory infections due to swelling around an already narrow airway.
Investigations
A high index of suspicion is needed to diagnose vascular airway compression. Key investigations include:
- Flexible Bronchoscopy
Gold standard for assessing dynamic airway collapse. Visualizes exact site and severity of compression and helps
differentiate from tracheomalacia or bronchomalacia. - CT Angiography / MRI Angiography
Defines vascular anatomy and relationship with airway. Essential for pre-surgical planning. - Echocardiography
Detects underlying congenital heart disease and assesses vascular dimensions. - Airway imaging (3D reconstruction)
Provides detailed airway dimension analysis. - Lung function tests (in older children)
Shows fixed or variable extrathoracic obstruction patterns.
Management
Conservative / Medical
- Monitoring in mild cases
- Treatment of associated tracheomalacia
- Respiratory physiotherapy
- Control of infections and minimizing airway inflammation
Surgical
- Vascular ring division
- LEEP (Left pulmonary artery anterior translocation) for pulmonary artery sling
- Aortopexy or Tracheopexy in severe tracheal collapse
- Slide tracheoplasty in long-segment stenosis
Postoperative bronchoscopy is often required to assess airway healing.
Prognosis
With early diagnosis and appropriate surgical correction, most children recover well and show
significant improvement in breathing, growth, and quality of life.
Conclusion
Vascular Airway Compression in children should be suspected when symptoms of wheezing, stridor, or recurrent pneumonia
do not improve with routine asthma therapy. Bronchoscopy and CT angiography are essential for diagnosis,
and timely intervention helps prevent long-term airway damage and improves outcomes.
Frequently Asked Questions (FAQs)
1. What causes vascular airway compression in children?
It is usually caused by abnormal development or enlargement of major blood vessels around the trachea or bronchi, such as vascular rings or pulmonary artery sling.
2. How is vascular airway compression diagnosed?
Diagnosis involves bronchoscopy, CT/MR angiography, and echocardiography to assess both airway narrowing and underlying vascular anomalies.
3. What symptoms should alert parents to possible airway compression?
Persistent stridor, wheezing, recurrent chest infections, breathing difficulty during feeding, or poor response to asthma medications.
4. Is surgery always required?
Not always. Mild cases may be monitored, but moderate to severe compressions typically require surgical correction for long-term improvement.
5. What is the long-term outcome after treatment?
Most children show excellent recovery, with improvement in breathing and reduction in infections after timely diagnosis and correction.