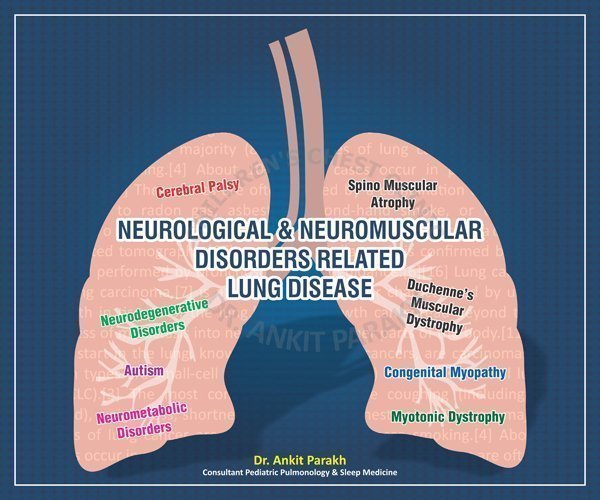
Neuromuscular/ Neurological Disorders Related Lung Diseases
How Neuromuscular Disorders Affect Breathing
Neuromuscular disorders affect the nerves and muscles, leading to weakened respiratory muscles. This can result in:
- Inefficient Breathing: Reduced strength in the diaphragm and intercostal muscles makes it harder to take deep breaths and expel carbon dioxide effectively.
- Reduced Airway Clearance: Weakened cough reflex increases the risk of mucus buildup and infections.
- Sleep-Disordered Breathing: Conditions such as obstructive sleep apnea (OSA) or hypoventilation are common due to poor muscle tone and airway collapse during sleep.
Common Respiratory Issues in Children with NMDs
- Chronic Hypoventilation: Inadequate breathing during sleep leads to low oxygen and high carbon dioxide levels.
- Recurrent Respiratory Infections: Impaired mucus clearance predisposes children to infections like pneumonia.
- Obstructive Sleep Apnea: Airway instability during sleep causes repeated episodes of airway obstruction, disrupting sleep quality.
The Role of Sleep in Neuromuscular Disorders
Sleep disturbances are prevalent in children with NMDs due to respiratory insufficiency and muscle weakness. Poor sleep can exacerbate fatigue, reduce cognitive function, and impair overall growth and development. Addressing these issues early is critical to maintaining a child’s overall well-being.
Key Diagnostic Tools
- Polysomnography (Sleep Study): Detects sleep-disordered breathing, including OSA and hypoventilation. For details on sleep study click here (https://www.ankitparakh.com/specialty-services/pediatric-sleep-studies/)
- Lung Function Tests: Measures lung capacity and respiratory muscle strength. For details of lung function tests click here (https://www.ankitparakh.com/specialty-services/pediatric-lung-function-testing/)
- Blood Gas Analysis: Identifies carbon dioxide retention, especially during sleep.
Management Strategies
- Non-Invasive Ventilation (NIV): Devices like BiPAP provide respiratory support, particularly during sleep.
- Airway Clearance Techniques:Suction devices, cough-assist machines, and physiotherapy help maintain clear airways.
- Regular Monitoring: Routine check-ups with a pediatric pulmonologist to track respiratory function and make timely adjustments.
- Nutritional Support: Adequate nutrition helps maintain muscle strength and immune function.
- Medication and Vaccination: Immunizations against respiratory infections and medications to manage symptoms like secretions.
Respiratory and sleep problems in children with Neuromuscular Disorders require a multidisciplinary approach involving pediatric pulmonologists, neurologists, and rehabilitation specialists. Early diagnosis, regular monitoring, and tailored interventions can significantly enhance the health and well-being of these children. If your child is having any neuromuscular disorder there is a high risk of having sleep and respiratory problems. It is highly recommended to be under the follow up of a pediatric neurologist and pediatric respiratory expert for optimal care.
Conclusion
Frequently Asked Questions (FAQs)
1. What are the most common neuromuscular disorders in children?
Conditions like Congenital Myopathies, Muscular Dystrophies, and Spinal Muscular Atrophy (SMA) are among the most frequently diagnosed.
2. How do neuromuscular disorders lead to breathing problems?
These disorders weaken the respiratory muscles, making it harder to breathe deeply, clear mucus, and maintain open airways during sleep.
3. What are the signs of sleep-disordered breathing in children with NMDs?
Snoring, restless sleep, morning headaches, excessive daytime sleepiness, and poor growth may indicate underlying sleep-disordered breathing.
4. How can non-invasive ventilation help?
NIV supports weakened respiratory muscles by providing positive airway pressure, improving oxygenation and reducing carbon dioxide retention during sleep.
5. How often should respiratory function be monitored in children with NMDs?
Routine evaluations every 3-6 months or as recommended by a pediatric pulmonologist are essential, especially during periods of rapid growth or illness.
6. Can children with NMDs lead a normal life with proper respiratory care?
With timely interventions and comprehensive care, many children with NMDs can achieve improved quality of life and participate in daily activities.



