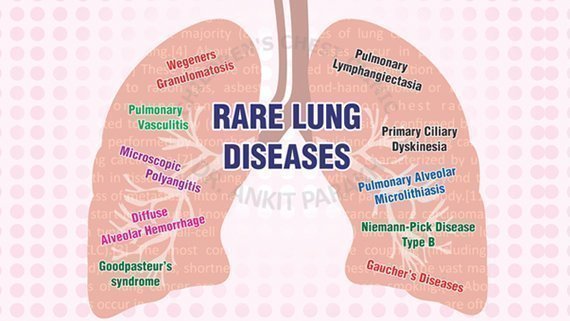
Rare Lung Disease
There are rare and complex lung diseases that can affect children, often requiring specialized care. These diseases can be difficult to diagnose and may have overlapping symptoms with more common conditions. As a pediatric pulmonologist, we encounter several rare lung diseases in practice, including Diffuse Alveolar Hemorrhage (DAH), Pulmonary Vasculitis, Primary Ciliary Dyskinesia (PCD), Interstitial Lung Diseases and Bronchiolitis Obliterans. In this section we shall briefly discuss these conditions, their symptoms, causes, and treatment options. Interstitial lung diseases are discussed in detail in a separate section.
1. Diffuse Alveolar Hemorrhage (DAH) in Children
Diffuse Alveolar Hemorrhage (DAH) refers to bleeding in the small air sacs (alveoli) in the lungs, which can impair the ability to exchange oxygen and carbon dioxide. This rare and serious condition is typically a result of inflammation in the lungs, and it may be associated with other underlying disorders like autoimmune diseases, infections, or certain drugs. Major symptoms of DAH in children include coughing up blood and difficulty breathing. Diagnosis involves imaging studies, such as chest X-rays or CT scans, along with a bronchoscopy to identify bleeding in the lungs. Treatment usually focuses on addressing the underlying cause of DAH, such as autoimmune disorders or infections, and may include medications like corticosteroids and immunosuppressants.
2. Pulmonary Vasculitis in Children
Pulmonary Vasculitis is a condition in which blood vessels in the lungs become inflamed. This inflammation can lead to severe damage to the lungs and other organs. Pulmonary vasculitis is often part of a larger systemic condition, such as Wegener’s Granulomatosis, Microscopic Polyangiitis or Churg-Strauss Syndrome, and can result in significant lung dysfunction. Children with pulmonary vasculitis may present with shortness of breath, persistent cough and coughing up blood. Diagnosing pulmonary vasculitis often involves blood tests, imaging, and sometimes a lung biopsy. The treatment plan typically includes high-dose corticosteroids and immunosuppressive drugs to control the inflammation and prevent further damage.
3. Primary Ciliary Dyskinesia (PCD)
Primary Ciliary Dyskinesia (PCD) is a rare genetic disorder that affects the cilia—tiny hair-like structures in the respiratory tract. The cilia normally move in a coordinated manner to clear mucus and other debris from the airways. In PCD, the cilia either don’t move correctly or don’t move at all, leading to mucus buildup and chronic respiratory issues. Symptoms of PCD in children often include chronic cough, recurrent respiratory infections (e.g., pneumonia, sinusitis), ear infections and hearing loss. Diagnosing PCD typically involves tests that assess ciliary function, such as nasal nitric oxide testing, electron microscopy of cilia, and genetic testing. Management of PCD focuses on preventing infections and clearing mucus from the airways through treatments such as chest physiotherapy, inhaled medications, and sometimes antibiotics to treat infections.
4. Bronchiolitis Obliterans in Children
Bronchiolitis Obliterans is a rare, severe form of chronic obstructive pulmonary disease (COPD) in children, often resulting from viral infections like adenovirus, or as a consequence of post-transplant complications or toxic inhalation. This condition involves inflammation and scarring of the bronchioles (the small airways in the lungs), leading to airway obstruction and decreased lung function. Symptoms of bronchiolitis obliterans may include chronic cough, persistent wheezing, difficulty breathing. Treatment for bronchiolitis obliterans may include corticosteroids, bronchodilators, and supportive respiratory therapy. In severe cases, lung transplantation may be necessary.
Treatment Approaches for Rare Lung Diseases in Children
Treatment for rare lung diseases in children varies depending on the specific diagnosis and underlying cause. The general approach includes:
- Medications: Corticosteroids, immunosuppressive drugs, and antibiotics are commonly used to control inflammation and manage infections.
- Supportive Care: Oxygen therapy and mechanical ventilation may be necessary for children with severe respiratory distress.
- Pulmonary Rehabilitation: Physical therapy and breathing exercises can help children improve lung function and manage chronic symptoms.
- Surgical Interventions: In some cases, lung surgery or a lung transplant may be considered for children with severe or progressive lung disease.
Rare lung diseases in children, such as Diffuse Alveolar Hemorrhage, Pulmonary Vasculitis, Primary Ciliary Dyskinesia, and Bronchiolitis Obliterans can be challenging to diagnose and manage. However, with early intervention and appropriate care, children with these conditions can often lead active lives.
Conclusion
Frequently Asked Questions (FAQs)
1. What is Diffuse Alveolar Hemorrhage (DAH) in children?
Diffuse Alveolar Hemorrhage is a rare condition where bleeding occurs in the small air sacs (alveoli) of the lungs. It is often associated with autoimmune diseases or infections and requires immediate medical attention to prevent respiratory failure.
2. How is Pulmonary Vasculitis diagnosed in children?
Pulmonary Vasculitis is diagnosed through a combination of blood tests, imaging (such as chest X-rays or CT scans), and, in some cases, a lung biopsy. The condition is often linked with systemic autoimmune diseases.
3. What are the symptoms of Primary Ciliary Dyskinesia (PCD) in children?
Children with PCD often experience chronic respiratory infections, a persistent cough, ear infections, and hearing loss. The condition is due to defective cilia that cannot effectively clear mucus from the airways.
4. Can ILD associated with systemic disorders be treated?
Yes, ILD associated with systemic disorders can be treated. Treatment typically includes medications such as corticosteroids and immunosuppressants to control inflammation and prevent further lung damage. In some cases, more advanced treatments like lung transplants may be necessary.
5. What is Bronchiolitis Obliterans and how is it treated?
Bronchiolitis Obliterans is a severe lung condition that involves the obstruction of small airways due to inflammation and scarring. It may be caused by viral infections or post-transplant complications. Treatment may include corticosteroids, bronchodilators, and, in some cases, lung transplantation.



