Necrotizing Pneumonia in Children
Necrotizing Pneumonia is a severe and increasingly recognized complication of pneumonia in children, characterised by progressive destruction of lung tissue leading to cavitation and sometimes pulmonary gangrene. Despite being uncommon, it is associated with significant morbidity and prolonged hospital stay. Early recognition and appropriate management are essential for improved outcomes.
Aetiology & Underlying Causes
Necrotizing Pneumonia develops when severe bacterial pneumonia causes reduced blood supply to lung tissue, leading to tissue necrosis. Common causative organisms include:
- Streptococcus pneumoniae – most frequent cause
- Staphylococcus aureus (including MRSA)
- Group A Streptococcus
- Mycoplasma pneumoniae
- Less commonly: Gram-negative bacteria, viral infections (Influenza, COVID-19) predisposing to bacterial coinfection
Risk Factors
- Inadequately treated or severe pneumonia
- Immunodeficiency disorders
- Viral lower respiratory tract infection preceding bacterial pneumonia
- Malnutrition
- Chronic lung disease or aspiration
Clinical Presentation
Children with Necrotizing Pneumonia typically present with symptoms similar to severe pneumonia, but with poorer response to treatment:
- High-grade fever persisting despite antibiotics
- Rapid or difficult breathing (respiratory distress)
- Chest pain or pleuritic pain
- Persistent toxicity or lethargy
- Decreased appetite and weight loss
- Signs of complications such as empyema, pneumothorax, or sepsis
Investigations
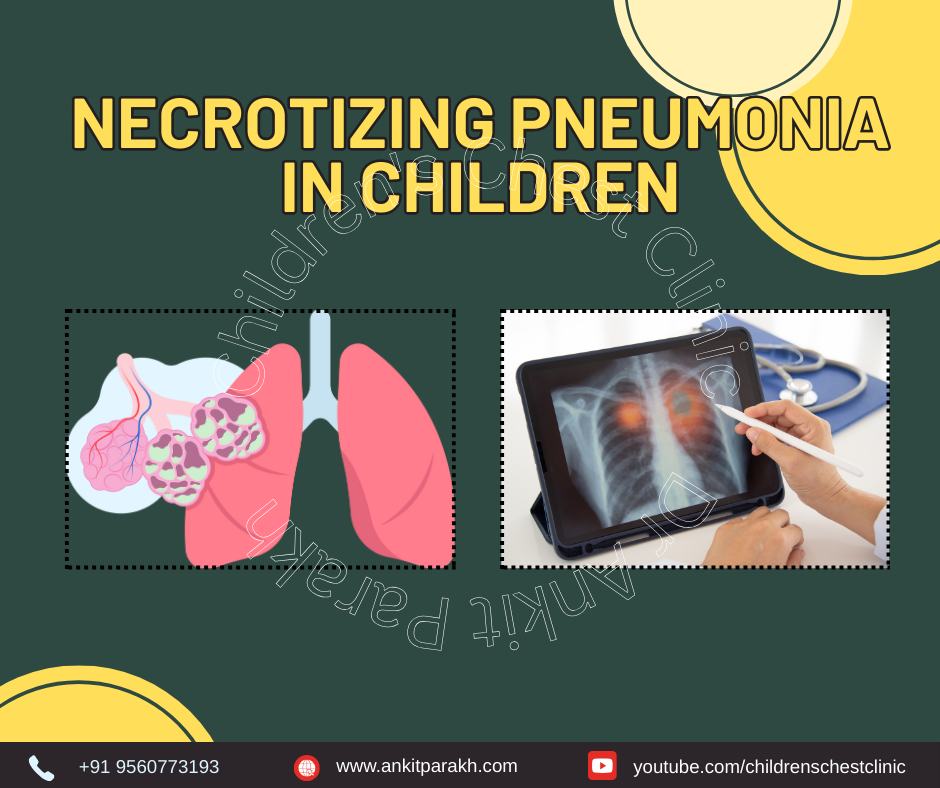
Diagnostic Evaluation
- Chest X-ray – may show multilobar consolidation, air-fluid levels, or cavities
- Chest CT scan – gold standard for confirming lung necrosis and cavitation
- Ultrasound chest – evaluates pleural effusion, empyema, and loculations
- Blood tests – CBC, CRP, ESR, Procalcitonin, blood culture
- Pleural fluid analysis if empyema present
- Bronchoscopy – for airway clearance or sample collection in selected cases
Treatment & Management
Management of Necrotizing Pneumonia focuses on prolonged antibiotics and supportive care.
1. Antibiotics
- Broad-spectrum IV antibiotics targeting common organisms
- Coverage adjusted based on culture sensitivity
- Duration typically 3–6 weeks
2. Supportive Care
- Oxygen therapy
- Adequate hydration
- Analgesia and antipyretics
- Chest physiotherapy
3. Management of Complications
- Drainage of empyema using chest tube or VATS (video-assisted thoracoscopic surgery)
- Mechanical ventilation if severe respiratory failure
- Rarely, surgical resection is required for persistent lung infection
4. Follow-up & Prognosis
Most children recover well with appropriate treatment, though radiological healing may take months. Long-term outcomes are typically good with minimal residual lung damage.
Prevention
- Timely treatment of pneumonia
- Vaccination – Pneumococcal and Influenza vaccines
- Early medical attention for persistent fever or breathing difficulty
Conclusion
Necrotizing Pneumonia is a serious complication of pneumonia in children that requires early recognition and aggressive management. Awareness of its presentation and prompt referral to a pediatric pulmonologist can substantially improve outcomes.