Multidrug-Resistant Tuberculosis (MDR TB) in Children
Multidrug-resistant tuberculosis (MDR TB) is a serious form of tuberculosis that does not respond to at least isoniazid and rifampicin—the two most powerful anti-TB medicines. Treating MDR TB in children requires a specialized approach that balances efficacy, safety, and child-specific considerations such as growth, nutrition, and adherence.
What is MDR TB?
MDR TB develops when the bacteria causing tuberculosis become resistant to the standard first-line drugs. This may occur due to incomplete or irregular TB treatment, drug misuse, or transmission from an adult with resistant TB. In children, infection usually occurs through close contact with an infected adult, making early detection and preventive measures crucial.
Diagnosis of MDR TB in Children
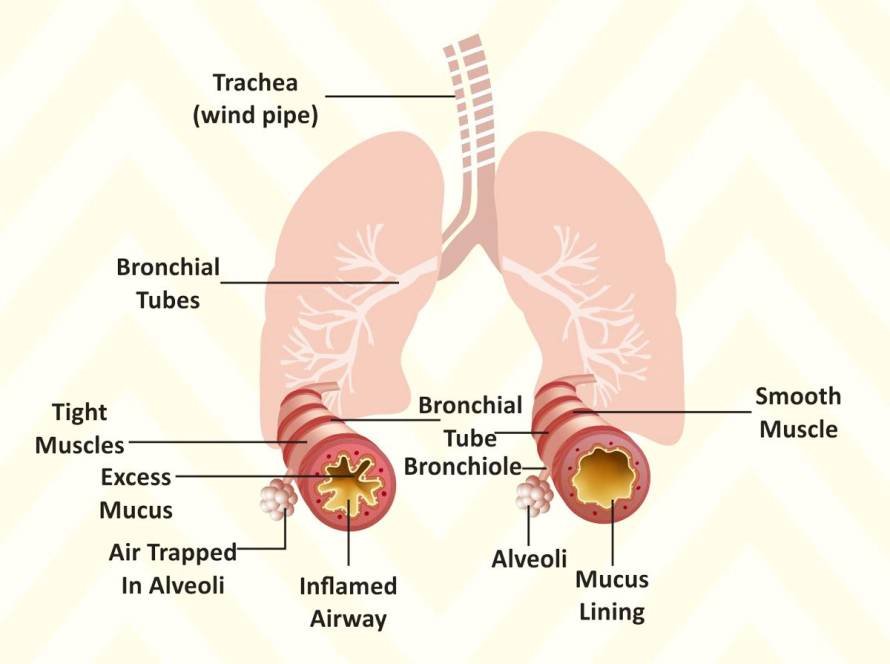
Diagnosing MDR TB in children is challenging due to their typically lower bacterial load and difficulty in obtaining sputum samples.
- Modern diagnostic tools such as GeneXpert MTB/RIF, line probe assays (LPA), and culture-based drug susceptibility testing (DST) are used to confirm resistance patterns.
- Clinical assessment, imaging (like chest X-rays), and history of contact with an MDR TB case are also important clues.
Treatment of MDR TB in Children
The treatment of MDR TB in children is individualized based on drug resistance patterns and national guidelines.
Key principles include:
1) Use of Second-Line Anti-TB Drugs
Children with MDR TB are treated with a combination of second-line drugs. The newer all-oral, shorter MDR TB regimens are now preferred to avoid painful injectable medications and minimize toxicity.
Typical drug groups include:
- Fluoroquinolones (Levofloxacin, Moxifloxacin)
- Bedaquiline and Delamanid (newer agents improving outcomes)
- Linezolid, Clofazimine, and Cycloserine
- Pyrazinamide and Ethambutol (if still effective)
2) Duration of Therapy
Treatment usually lasts 9 to 18 months, depending on the drug regimen and response. Shorter regimens (9–11 months) may be used for eligible cases, improving compliance and outcomes.
3) Monitoring and Management of Side Effects
Children require close monitoring for potential side effects such as:
- Gastrointestinal upset
- Hearing loss
- Peripheral neuropathy
- QT interval prolongation (with bedaquiline)
Regular clinical reviews, laboratory tests, and ECG monitoring help ensure safety.
4) Nutritional and Psychological Support
Malnutrition worsens TB outcomes. Nutritional supplementation and family counselling play vital roles in recovery. Emotional support helps children cope with the long duration and possible stigma of treatment.
5) Adherence and Follow-Up
Adherence to treatment is critical to prevent further resistance and relapse. Directly Observed Therapy (DOT) and caregiver education ensure regular medication intake. After completion, follow-up for at least 12 months is advised to detect any relapse early.
Outcomes and Prognosis
With early diagnosis, proper drug selection, and multidisciplinary care, most children with MDR TB can be successfully treated. The success rate exceeds 80% in well-managed cases, highlighting the importance of specialized pediatric TB care.
Key Takeaways
- MDR TB in children is treatable with new, all-oral regimens.
- Early diagnosis using molecular tests is essential.
- Nutritional, psychological, and adherence support significantly improve outcomes.
- New drugs like bedaquiline and delamanid have transformed MDR TB treatment in children.
Frequently Asked Questions (FAQs)
1. What causes MDR TB in children?
MDR TB in children usually occurs after exposure to an adult with drug-resistant TB or due to incomplete treatment of earlier TB infection.
2. How long is the treatment for MDR TB in children?
Treatment typically lasts 9–18 months, depending on the resistance pattern and the regimen used.
3. Is MDR TB contagious among children?
Yes, MDR TB can spread from person to person through air, but children are generally less infectious than adults.
4. Are new drugs available for MDR TB in children?
Yes, newer medications like bedaquiline and delamanid are now approved for use in children, offering safer and more effective all-oral options.
5. Can MDR TB in children be cured completely?
Yes. With timely diagnosis, appropriate treatment, and good adherence, most children with MDR TB achieve complete cure and lead healthy lives.