Atopic Dermatitis in Children
What is Atopic Dermatitis?
Atopic dermatitis is a chronic inflammatory skin condition that frequently starts during infancy or early childhood. It is often associated with other allergic conditions, such as asthma and allergic rhinitis. The condition tends to follow a relapsing and remitting course, meaning symptoms may flare up and subside periodically.
Symptoms of Atopic Dermatitis in Children
Common symptoms include:
- Dry, scaly skin: The common areas involved are the hands, feet, ankles, wrists, neck, upper chest, eyelids, inside the bend of elbows/knees in children. In infants, the face, extensor surfaces of arms/legs and scalp as more involved.
- Intense itching: Scratching can worsen the condition and lead to skin infections.
- Redness and inflammation: Often seen in affected areas during flare-ups.
- Skin thickening: Caused by repeated scratching over time.
The condition can vary in severity, from mild to severe, affecting the child’s sleep, mood, and daily activities.
Causes and Triggers
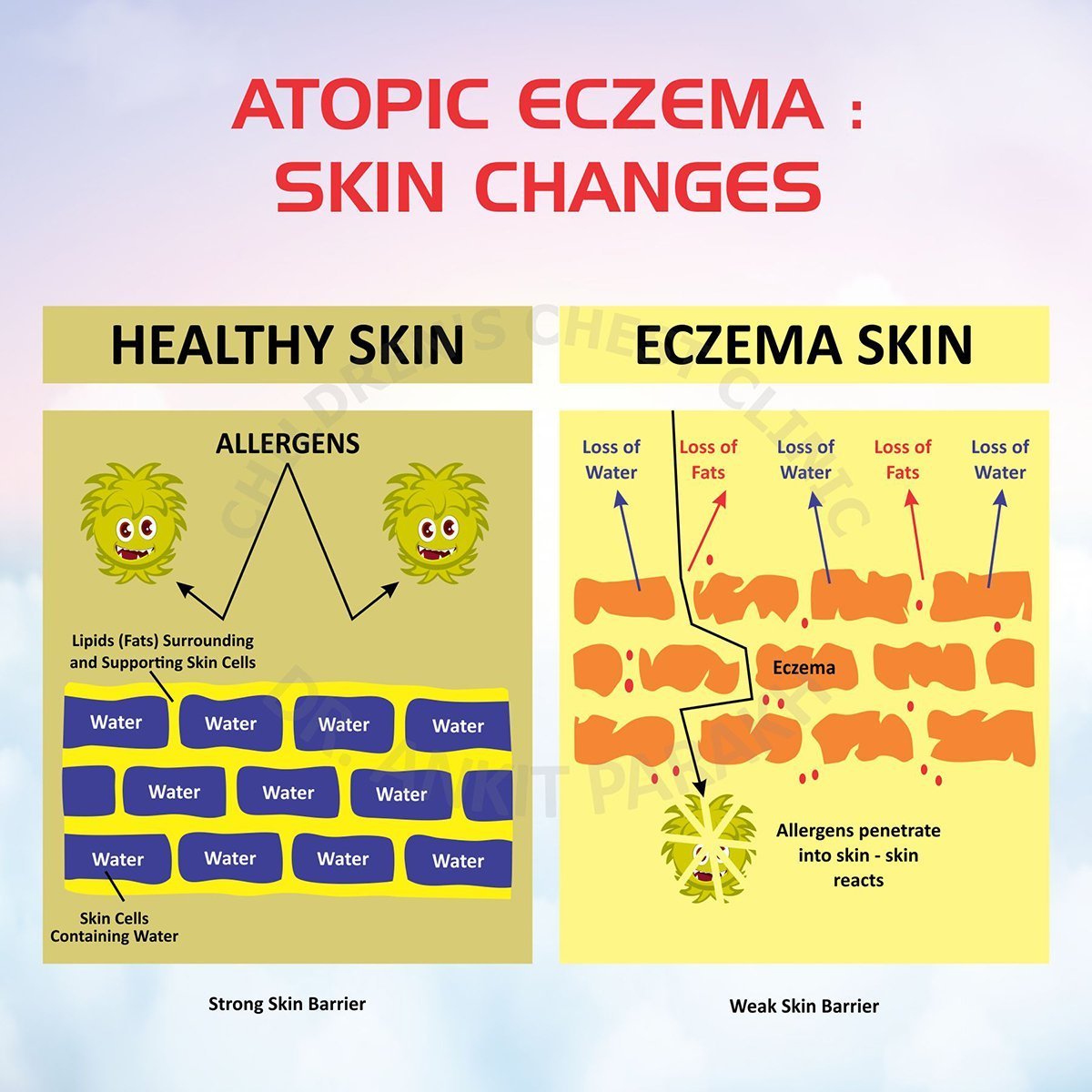
Atopic dermatitis results from a combination of genetic and environmental factors. The skin’s barrier is compromised, leading to dryness and increased susceptibility to irritants and allergens. Common triggers include:
- Irritants: Soaps, detergents, and perfumes.
- Allergens: Dust mites, pollen, and pet dander.
- Climate: Dry or cold weather can worsen symptoms.
- Food Allergies: Some children may experience flares linked to certain foods.
Managing Atopic Dermatitis
- Moisturisers: Keeping the skin hydrated is essential. Use thick, fragrance-free moisturisers multiple times a day, especially after bathing, to restore the skin barrier.
- Bathing: Bathing should be gentle and brief (5-10 minutes) in lukewarm water. Avoid harsh soaps and opt for mild, soap-free cleansers. Pat the skin dry and immediately apply moisturisers to lock in moisture.
- Topical Calcineurin Inhibitors: Topical calcineurin inhibitors like tacrolimus and Pimecrolimus are commonly used non steroid drugs for management of allergic dermatitis in children.
- Wet Wraps: This involves applying moisturisers and topical steroids (if advised) and wrapping the affected areas with wet bandages. Wet wraps are particularly effective for severe flares as they help hydrate the skin and calm inflammation.
- Avoiding Triggers: Identifying and avoiding triggers is critical in preventing flare-ups. Allergy testing may be recommended in some cases.
Eczema Action Plan
This is a written one-page document which provides key information on how to treat your child as the eczema changes. It provides information on the daily bathing advice and moisturizer to be used, what to do when there is a flare and when to consult your doctor. Every child with atopic eczema should have an eczema action plan!
Complications of Atopic Dermatitis
The most common complication of atopic eczema is a bacterial skin infection. Children with atopic eczema have a cracked and broken skin. This increase the risk of the skin getting infected with bacteria. With superadded bacterial infections the skin becomes more red, hot, swollen, sore and develops oozing of pus. Early treatment with topic or oral antibiotic is required in such situations. Bleach baths can be quite helpful in children getting frequent skin infections
The other common complications are viral skin infections such as herpes viral infections. Apart form these various other complications are seen such as sleeping problem because of excessive itching, poor self confidence, psycological issues and bullying in school.
Atopic dermatitis can be challenging to manage, but with a comprehensive approach involving moisturisers, proper bathing routines, topical steroids, topical calcineurin inhibitors and wet wraps, children can experience significant relief.
If your child is having atopic dermatitis or eczema consult a pediatric allergist who can guide you on effective treatment plans tailored to your child’s needs.
Conclusion
Frequently Asked Questions (FAQs)
1. Is atopic dermatitis the same as eczema?
Yes, eczema is a general term for skin inflammation, and atopic dermatitis is the most common type of eczema in children.
2. What are eczema flares?
Children with atopic dermatitis can have times when the skin turns red, hot, burning, crusted or “weepy” and more itchy. These phases are called as flares. During times of flares the child would need a steroid cream to be applied in addition to the moisturizer.
3. Are moisturisers enough to treat atopic dermatitis?
Moisturisers are crucial for maintaining the skin barrier, but additional treatments like topical steroids or topical calcineurin inhibitors may be needed depending on the severity of the eczema.
4. Can certain foods worsen eczema in children?
In some children atopic dermatitis and food allergies are related. In children with severe infantile eczema and poor response, allergy to milk and egg should be considered. Consult an allergist if you suspect food is a trigger.
5. Is daily bathing harmful for children with eczema?
No, daily bathing is beneficial if followed by immediate application of moisturisers. It helps hydrate and cleanse the skin when done correctly. Make your baby bathe in luke warm water with a very mild soap or a non-soap cleanser. After bath, gently pat skin dry (avoid rubbing the skin) to keep it moist or slightly wet. Apply moisturizer right away on the wet skin to retain the moisture. This is called as ‘Soak and Seal Technique’.



