Tuberculosis in Children: An Overview
Incidence of Tuberculosis in Children
According to the World Health Organization (WHO), an estimated 1.1 million children develop TB each year, accounting for 11% of all TB cases globally. While TB is more prevalent in adults, children are at higher risk of developing severe forms, such as TB meningitis and miliary TB.
- High-Burden Regions: Countries in South Asia, Africa, and Southeast Asia have a higher prevalence of childhood TB due to endemic TB and socio-economic factors.
- At-Risk Groups: Infants, malnourished children, and those with compromised immunity (e.g., HIV-infected children) are at increased risk.
How Does Tuberculosis Spread?
TB is caused by Mycobacterium tuberculosis and primarily spreads through airborne droplets. When an infected person with pulmonary TB coughs, sneezes, or speaks, the bacteria are released into the air.
- Close Contact: Children often contract TB from close household contacts, such as parents or caregivers with active TB.
- Latent Infection: After inhaling TB bacteria, the infection may remain latent, causing no symptoms but posing a risk of future reactivation, especially in immune-compromised children.
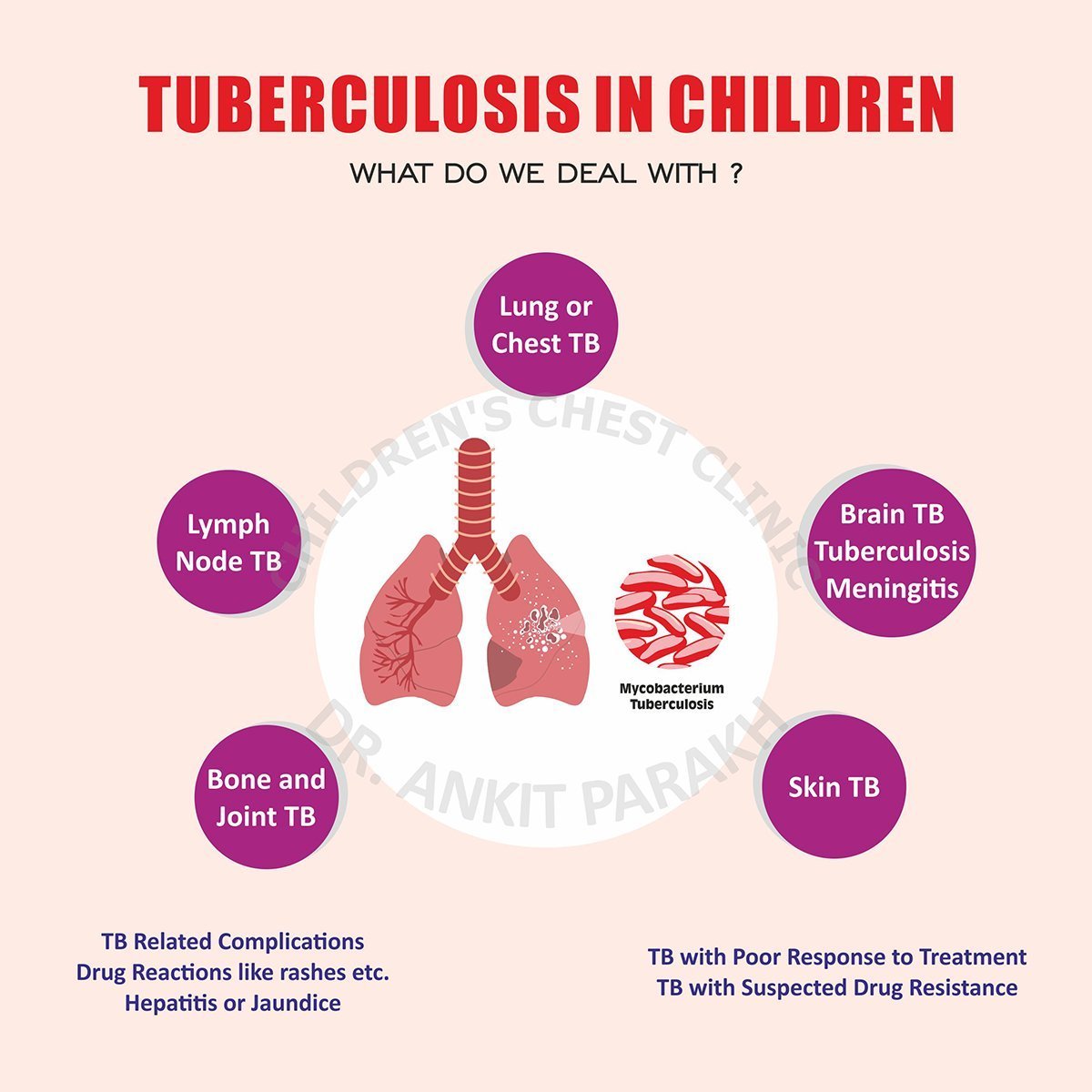
Sites of Tuberculosis in Children
TB can affect multiple organs in children, with pulmonary TB being the most common.
- Pulmonary Tuberculosis: Affects the lungs and presents with symptoms like persistent cough, fever, and weight loss.
- Lymph Node TB (Tuberculous Lymphadenitis): Enlarged lymph nodes, commonly in the neck, are a hallmark of this extrapulmonary form.
- Abdominal TB: Involves the intestines, peritoneum, or abdominal lymph nodes, leading to abdominal pain, swelling, or altered bowel habits.
- TB Meningitis: A severe form affecting the brain and meninges, causing headaches, vomiting, seizures, or altered consciousness.
- Bone and Joint TB: Affects the spine (Pott’s disease) or large joints, leading to pain, swelling, or restricted movement.
- Miliary TB: Disseminated TB affecting multiple organs, often presenting with fever, weight loss, and severe systemic symptoms.
Importance of Early Diagnosis
Early detection and treatment of TB in children are crucial to prevent complications and transmission. Delayed diagnosis can lead to severe forms of TB that are harder to treat and may result in long-term health issues.
Preventing Tuberculosis in Children
- BCG Vaccination: Administered at birth, it provides protection against severe TB forms.
- Contact Tracing: Screening household members of TB patients helps detect latent or active TB early.
- Infection Control: Avoiding close contact with individuals with active TB reduces the risk of transmission.
Tuberculosis in children is a preventable and treatable condition with early detection, proper management, and preventive measures. Parents and caregivers should be vigilant about symptoms, particularly if the child has been in contact with someone diagnosed with TB. Consulting a pediatric specialist is crucial for accurate diagnosis and timely intervention.
Conclusion
Related Video
Frequently Asked Questions (FAQs)
1. How common is tuberculosis in children?
Tuberculosis affects an estimated 1.1 million children globally each year, with higher rates in regions with endemic TB.
2. How does tuberculosis spread in children?
TB spreads through airborne droplets when a person with active pulmonary TB coughs or sneezes. Children often contract TB from close household contacts.
3. What organs can tuberculosis affect in children?
TB can affect the lungs, lymph nodes, abdomen, brain (TB meningitis), bones, joints, or multiple organs in disseminated TB.
4. How is childhood tuberculosis diagnosed?
Diagnosis involves a combination of tests, including chest X-rays, tuberculin skin tests, blood tests, and advanced methods like GeneXpert.
5. Can tuberculosis in children be prevented?
Yes, through BCG vaccination, contact tracing, and reducing exposure to individuals with active TB, tuberculosis in children can be prevented.



