Abdominal Tuberculosis in Children: Causes, Symptoms, and Treatment
What is Abdominal Tuberculosis?
Abdominal tuberculosis refers to TB infection within the abdominal cavity. It can involve:
- Abdominal Lymph Nodes: The most common form, particularly affecting mesenteric lymph nodes.
- Peritoneal Tuberculosis: Involves the lining of the abdominal cavity, leading to ascites (fluid buildup).
- Gastrointestinal TB: Affects the intestines, most commonly the ileum and cecum.
- Solid Organ TB: Rarely, it can involve the liver, spleen, or pancreas. Usually multiple sites can be involved at a time.
Causes and Risk Factors
Abdominal tuberculosis is caused by Mycobacterium tuberculosis, which spreads through:
- Hematogenous (bloodstream) spread from a primary TB site, usually the lungs.
- Ingestion of infected sputum or contaminated milk in rare cases.
- Lymphatic spread, leading to abdominal lymph node involvement.
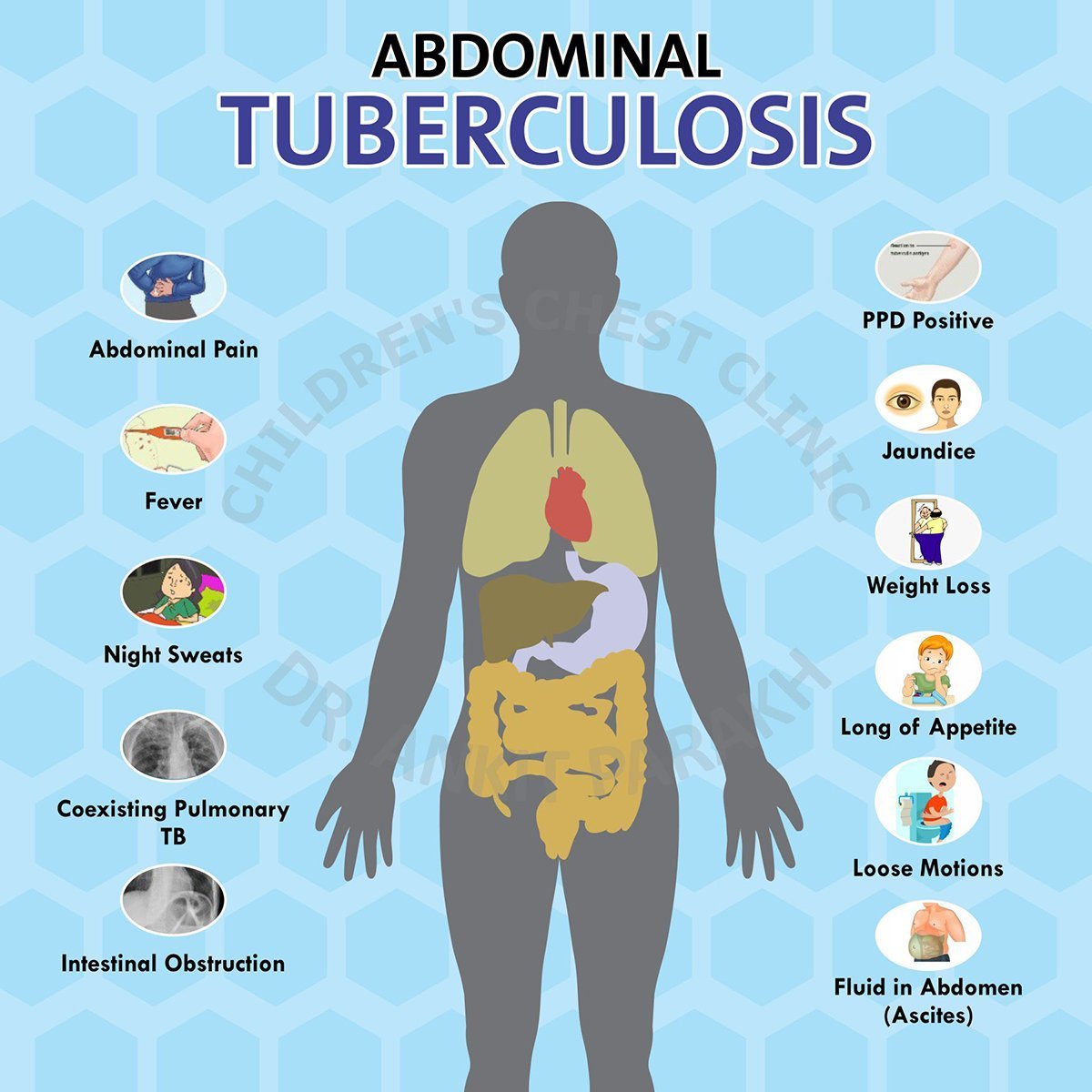
Symptoms of Abdominal Tuberculosis in Children
Symptoms can vary depending on the affected area but often include:
- Persistent abdominal pain or discomfort.
- Abdominal swelling or a palpable mass.
- Fever and night sweats.
- Weight loss and poor appetite.
- Altered bowel habits, such as diarrhea or constipation.
- In severe cases, intestinal obstruction or perforation.
Diagnosing Abdominal Tuberculosis
Accurate diagnosis involves a combination of clinical evaluation, imaging studies, and laboratory tests:
- Imaging: Ultrasound or CT scan can reveal enlarged abdominal lymph nodes, thickened intestinal walls, or ascitic fluid.
- Tuberculin skin test or IGRA to detect TB infection.
- Analysis of ascitic fluid for elevated protein levels, lymphocyte predominance, and ADA (adenosine deaminase) levels.
- Biopsy: Lymph node or intestinal biopsy may confirm the presence of TB granulomas.
- Molecular Tests: GeneXpert or PCR for Mycobacterium tuberculosis.
Treatment of Abdominal Tuberculosis
- Anti-Tuberculosis Therapy (ATT): A 6–9 month regimen of TB medications forms the cornerstone of treatment.
- Nutritional Support: Adequate nutrition to aid recovery and boost immunity.
- Surgery: Required in complicated cases, such as intestinal obstruction, perforation, or abscess formation.
Prognosis
With timely diagnosis and proper treatment, children with abdominal tuberculosis have a good prognosis. However, delayed treatment can lead to complications and long-term health issues.
Frequently Asked Questions (FAQs)
1. What causes abdominal tuberculosis in children?
It is caused by Mycobacterium tuberculosis, which spreads from the lungs or other primary TB sites to the abdominal cavity.
2. How is abdominal tuberculosis diagnosed?
Diagnosis involves imaging studies (e.g., ultrasound, CT scan), fluid analysis, biopsy, and molecular tests like GeneXpert.
3. Can abdominal tuberculosis be cured?
Yes, with a complete course of anti-tuberculosis therapy, most children recover fully.
4. What are the signs of abdominal lymph node involvement in TB?
Signs include abdominal pain, swelling, and sometimes a palpable mass in the abdomen.
5. What are the characteristics of lymph nodes in the abdomen which suggest tuberculosis?
Small lymph nodes up to less than 2 cm in size can be normally found inside the abdomen of children. Large lymph nodes more than 2 cm especially if multiple, conglomerate or mattered and necrotic are suggestive of tuberculosis.



