Pulmonary Tuberculosis in Children
What is Pulmonary Tuberculosis?
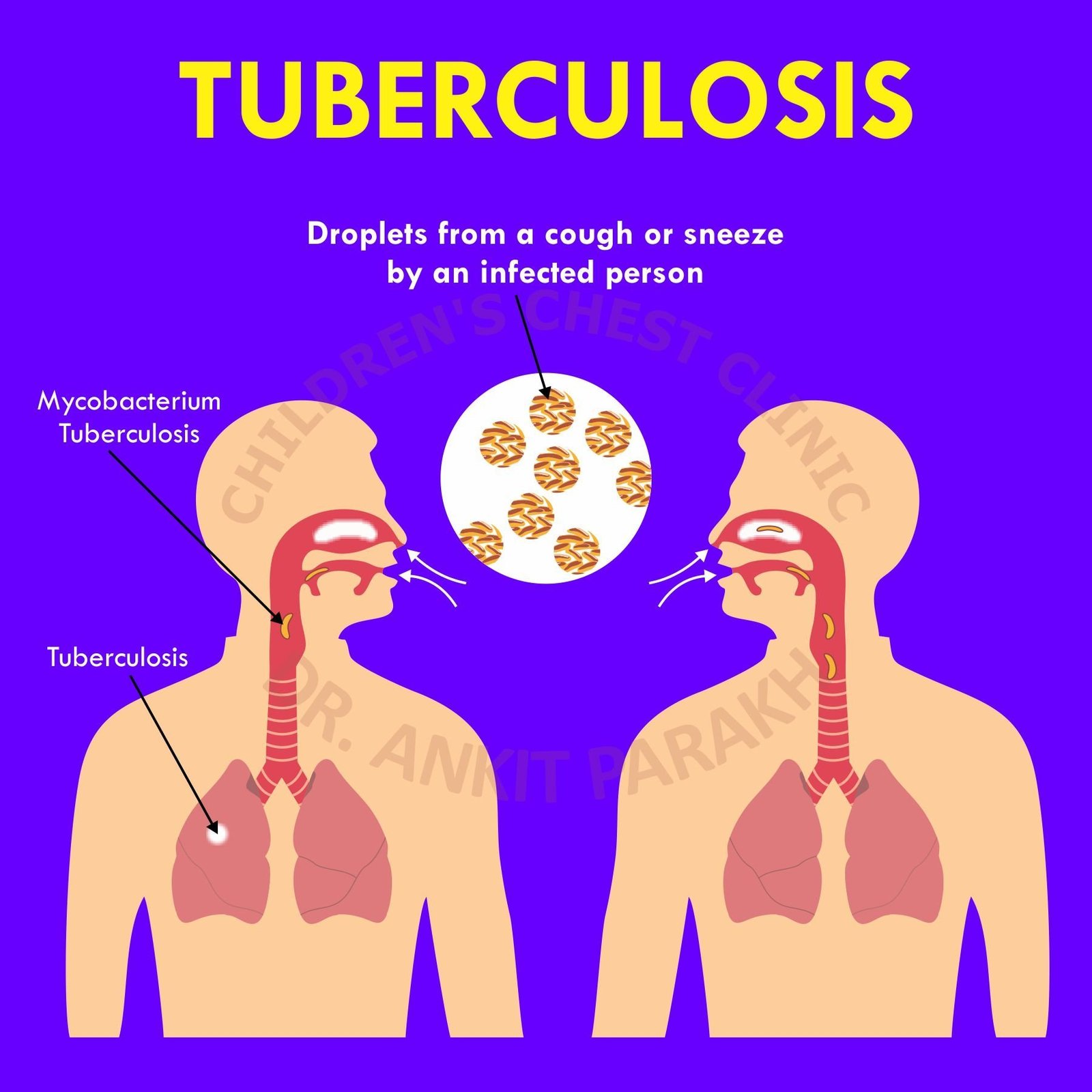
Pulmonary TB refers to tuberculosis infection localized in the lungs. It spreads through airborne droplets when an infected person coughs, sneezes, or speaks. Children usually contract TB from close contact with an adult who has active pulmonary TB.
Symptoms of Pulmonary TB in Children
Symptoms of pulmonary TB can vary based on the severity of the infection and the child’s immune status. Common symptoms include:
Diagnosis of Pulmonary TB in Children
Diagnosing pulmonary TB in children can be challenging due to their inability to produce sputum easily and the non-specific nature of symptoms. However, the following diagnostic tools help identify the disease:
- Chest X-Ray: Shows abnormalities such as consolidation, cavities, or enlarged lymph nodes in the lungs.
- Tuberculin Skin Test (TST): Measures the immune response to injected tuberculin. A positive result suggests TB infection but does not confirm active disease.
- Sputum Test: Sputum is sent for microbiological tests. The most reliable is the GeneXpert Tests. It is a molecular diagnostic test that detects TB bacteria and resistance to rifampicin. This test is highly accurate and widely used for diagnosing TB in children. Results are usually available in 1-2 days.
- Flexible Bronchoscopy: Used when sputum samples are difficult to obtain. A bronchoscope is inserted into the airways to collect samples directly from the lungs for analysis.
Treatment of Pulmonary TB in Children
- First-Line Anti-Tuberculosis Drugs: Treatment for drug-sensitive pulmonary TB includes a combination of isoniazid, rifampicin, pyrazinamide, and ethambutol during the initial intensive phase (2 months), followed by a continuation phase with isoniazid and rifampicin (4 months).
- Adherence to Medication: Directly Observed Therapy (DOT) ensures children complete the full course of treatment to prevent relapse or drug resistance.
- Supportive Care: Nutritional support is critical for recovery, as malnourished children are more susceptible to TB-related complications.
- Follow-Up: Regular monitoring through clinical assessments and weight tracking is essential to evaluate treatment progress.
Preventing Pulmonary TB in Children
- BCG Vaccination: Administered at birth, it provides protection against severe TB forms.
- Early Detection: Screen close contacts of TB patients, especially children, for early signs of infection.
- Infection Control: Minimize exposure to individuals with active TB, particularly in crowded settings.
Importance of Early Diagnosis
Children are at higher risk of developing severe TB forms, such as TB meningitis or miliary TB, if pulmonary TB is not diagnosed and treated promptly. Early intervention improves outcomes and prevents complications.
Pulmonary TB in children is a treatable and curable disease with early diagnosis and adherence to treatment. Parents and caregivers should be vigilant for symptoms, especially if the child has been in contact with someone diagnosed with TB. Pediatric pulmonologists and TB specialists play a vital role in ensuring effective diagnosis and management.
Conclusion
Frequently Asked Questions (FAQs)
1. What is pulmonary TB in children?
Pulmonary TB is a lung infection caused by Mycobacterium tuberculosis. It is the most common form of tuberculosis in children.
2. How is pulmonary TB diagnosed in children?
Diagnosis involves a combination of chest X-rays, GeneXpert tests, sputum examination and flexible bronchoscopy to confirm TB infection.
3. How does the GeneXpert test help in TB diagnosis?
The GeneXpert test detects TB bacteria and determines resistance to rifampicin, providing quick and accurate results.
4. What is the role of flexible bronchoscopy in TB diagnosis?
Most children with TB would present with pneumonia which is not improving with the usual medicines. In such cases flexible bronchoscopy is of immense help. Flexible bronchoscopy helps to have a direct airway examination and collect samples from the lungs.
5. Is all this detailed examination important or can we treat Tuberculosis (TB) on the basis of symptoms and Xrays?
This testing is very important since it would help confirm the disease and also let us know to which drugs the bacteria is sensitive. Drug resistance is increasing in our country and hence it is important that in all cases samples are sent for detailed analysis to the lab.




