Drug-Resistant Tuberculosis in Children: Causes, Challenges, and Treatment
What is Drug-Resistant Tuberculosis?
Drug-resistant tuberculosis occurs when the TB bacteria develop resistance to one or more anti-tuberculosis drugs. The most common forms include:
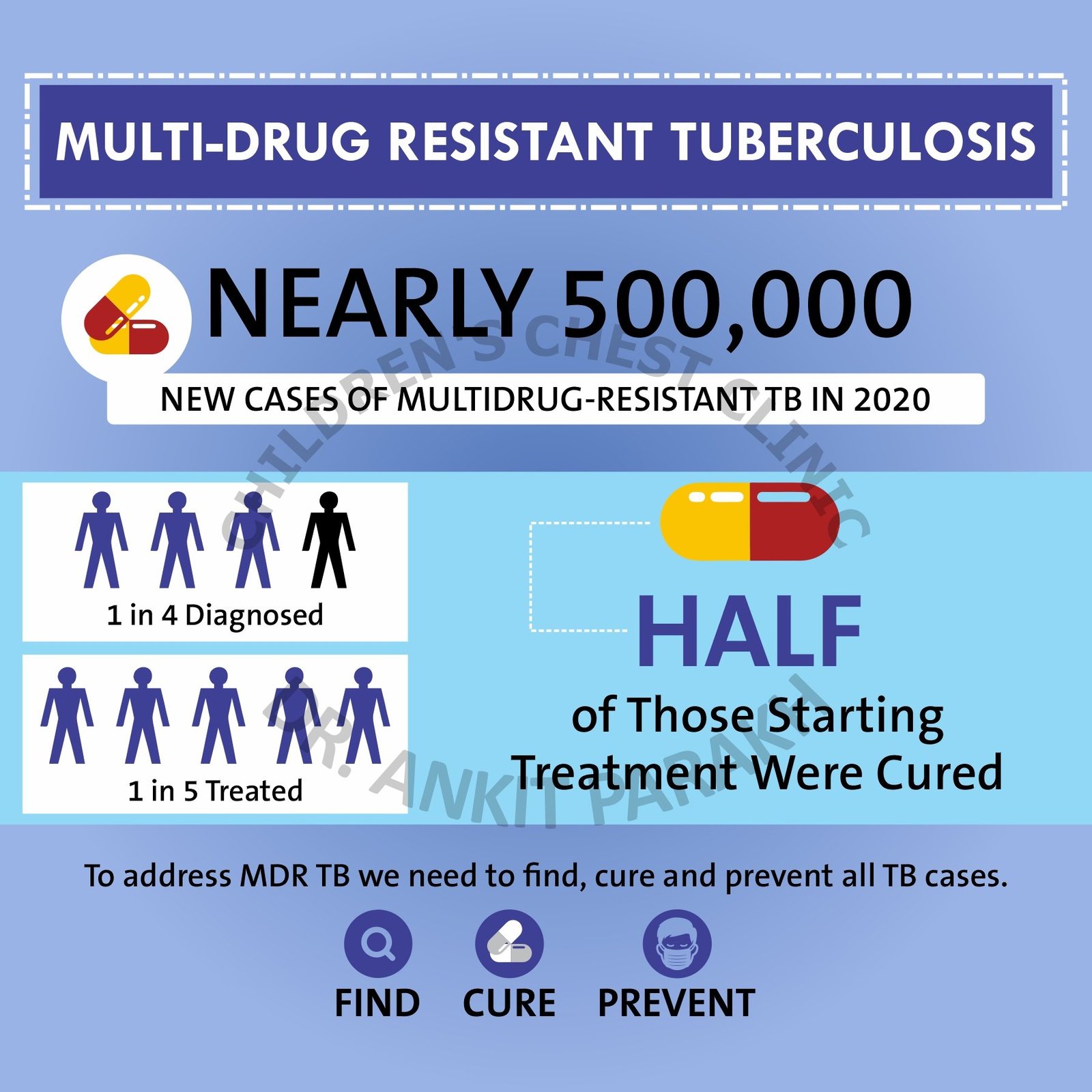
- Multidrug-Resistant TB (MDR-TB): Resistant to isoniazid and rifampicin, the two most effective first-line drugs.
- Extensively Drug-Resistant TB (XDR-TB): MDR-TB with additional resistance to fluoroquinolones and at least one second-line injectable drug.
Causes of Drug-Resistant Tuberculosis
- Incomplete Treatment: Interruptions in TB treatment or taking medications incorrectly.
- Direct Transmission: Infection with already resistant TB strains from another person.
- Improper Prescribing: Incorrect drug regimens or dosages.
- Weakened Immune Systems: In children with malnutrition, HIV, or other immune-compromising conditions, TB bacteria can develop resistance more easily.
Symptoms of Drug-Resistant TB in Children
Symptoms of DR-TB are often similar to drug-sensitive TB but may persist or worsen despite treatment. Common symptoms includes:
- Persistent cough
- Fever and night sweats
- Weight loss or failure to gain weight
- Fatigue and weakness
- Symptoms of specific organ involvement, such as swollen lymph nodes or abdominal pain, if extrapulmonary TB is present.
When should a Drug Resistance be considered?
Drug resistance should be considered in the following circumstances:
- Poor response to first line therapy: Poor response to treatment in a patient taking drugs as per a correct regime
- Treatment after lost to follow up (also called as Defaulter): child has already received TB medicines for at least one month and then has stopped treatment.
- Recurrent TB (Relapse): Child who been detected with TB in past and now has got a recurrence.
- Children in contact of MDR TB adult patients
Diagnosing Drug-Resistant Tuberculosis
Early and accurate diagnosis is essential for managing DR-TB. Diagnostic tools include:
- GeneXpert MTB/RIF: Detects TB bacteria and resistance to rifampicin.
- Line Probe Assay (LPA): Identifies resistance to first- and second-line drugs.
- MGIT TB Culture and Drug Susceptibility Testing (DST): Confirms Tb bacteria and drug resistance patterns to various TB drugs.
- GeneXpert XDR: Detects TB bacteria and resistance to many second line drugs.
Treatment of Drug-Resistant Tuberculosis in Children
The treatment of DR-TB is longer, more complex, and often involves medications with more side effects. Key aspects include:
Second-Line Drugs
- MDR-TB is treated with a combination of second-line drugs, including fluoroquinolones, bedaquiline, and linezolid.
- Treatment duration is typically 9–20 months, depending on the severity and drug resistance pattern.
Individualized Treatment Regimens
- Regimens are tailored based on drug susceptibility test results to ensure effectiveness.
Supportive Care
- Nutritional support and management of co-existing conditions, such as HIV or malnutrition, are crucial for successful outcomes.
Directly Observed Therapy (DOT)
- Ensures adherence to the lengthy treatment regimen, reducing the risk of further resistance.
Challenges in Treating Drug-Resistant Tuberculosis in Children
- Side Effects: Second-line drugs often cause side effects like nausea, hearing loss, and bone marrow suppression.
- Lengthy Treatment: The prolonged duration of treatment affects adherence.
- Stigma: Families may face social stigma, leading to delayed diagnosis and treatment.
Preventing Drug-Resistant Tuberculosis in Children
- Ensure completion of the full course of TB treatment in all cases.
- Screen close contacts of DR-TB patients for early detection.
- Improve infection control in healthcare and community settings.
- Encourage the use of BCG vaccination to protect against severe TB forms.
Drug-resistant tuberculosis in children is a serious condition requiring early diagnosis and meticulous treatment. With proper care and adherence to treatment protocols, many children can recover and lead healthy lives. If your child is suffering from tuberculosis do get in touch with a tuberculosis expert.
Conclusion
Frequently Asked Questions (FAQs)
1. What is drug-resistant tuberculosis?
Drug-resistant TB occurs when TB bacteria develop resistance to standard anti-tuberculosis medications, making treatment more difficult.
2. How do children develop drug-resistant TB?
Children may develop DR-TB due to incomplete treatment, direct transmission of resistant strains, or improper prescribing of medications.
3. How is drug-resistant TB treated in children?
Treatment involves second-line anti-TB drugs, tailored regimens, and supportive care, often lasting 9–20 months.
4. Can drug-resistant TB be cured in children?
Yes, with early diagnosis, effective treatment, and strict adherence, most children recover fully from DR-TB.
5. How can drug-resistant TB in children be prevented?
Preventive measures include completing TB treatment, screening close contacts, and maintaining infection control practices.



